February 25, 2024
For ventilation problems:
Spoon with light can save lives
In contrast to adults, ventilation is the most important measure in the resuscitation of children or in serious emergencies, because chest compressions alone are NOT suitable for children1! On the one hand, it is almost impossible for the small organism to survive without ventilation; on the other hand, there is a very high probability that the circulation will be reactivated quickly with ventilation!
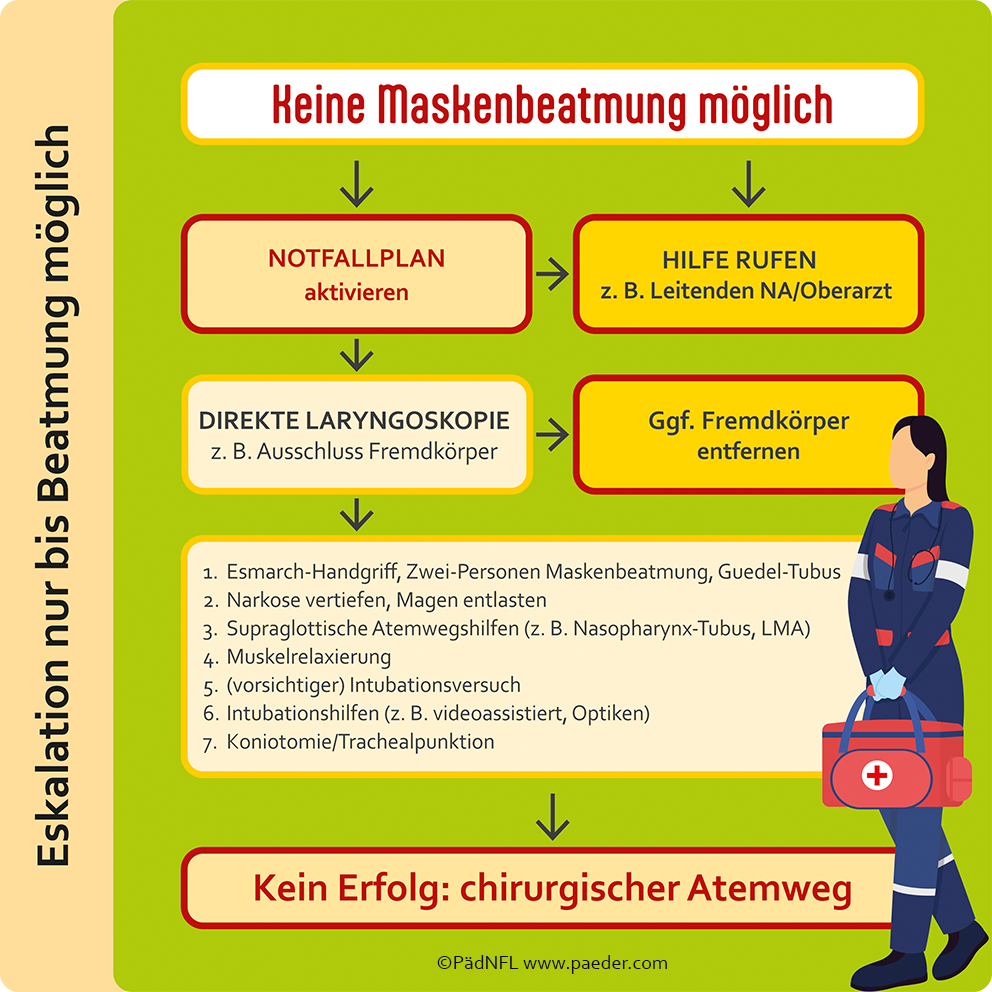
If mask ventilation is not successful, it is all the more important to know a clear course of action! I have shown it in this illustration:
The measures shown in the illustration should be escalated step by step from top to bottom until the child is successfully ventilated. The scheme shown largely corresponds to the recommendations of the Scientific Working Group on Pediatric Anesthesia (WAKKA) of the German Society of Anesthesiology and Intensive Care Medicine (DGAI)1,2. From my point of view and in my scheme, however, a laryngoscopy – especially preclinically – should be performed earlier than mentioned here in order to recognize a possible obstruction of the oropharynx with a foreign body or secretions. The laryngoscope is very valuable here, although the eponymous low position in front of the larynx, as in intubation, is not required. Often, simply opening and illuminating the mouth can detect the problems mentioned and enable suction or grasping with Magill forceps. This is the reason why I refer to this instrument not as a laryngoscope but as a “spoon with light” during lectures and training courses.
Remember: Always look in the mouth early if there are ventilation problems! It is unlikely that ventilation will not be possible if the measures shown are implemented immediately and in full, at the latest when the laryngeal mask is used. Based on my own experience, I do not agree with the WAKKA recommendations that invasive procedures (coniotomy, tracheostomy, surgical airway) are never necessary. A puncture coniotomy is not easy to perform on small children and infants, as this is the narrowest part of the child’s airway. The short neck forces the user to make a very steep puncture3,4. Therefore, a puncture tracheostomy – also difficult – should rather be attempted, in which a shallower puncture can be made and the trachea offers a larger lumen 5,6. If at all possible, however, a surgical opening of the trachea should be preferred, which an experienced surgeon (including pediatric surgeons) can perform within a few minutes7. This is much easier than in adults, where the thyroid gland often causes difficulties along the way8.
Security in seconds
The pediatric emergency ruler (PädNFL) helps when it comes to the correct dosage of life-saving medication in a child emergency. It enables the length-related weight of the small patient to be estimated immediately and displays the corresponding dosage recommendations. In addition, the PedNFL provides an overview of suitable equipment and standard values at a glance according to the child’s height and weight. The PedNFL is the only medical aid in the world that has been proven to prevent 9 out of 10 incorrect doses9,10. It is therefore expressly recommended in the S2k guideline “Drug safety in pediatric emergencies “11.
Literature:
- Van de Voorde P, Turner NM, Djakow J et al. European Resuscitation Council Guidelines 2021: Paediatric Life Support. Resuscitation 2021; 161: 327-387, DOI: 10.1016/j.resuscitation.2021.02.015.
- Weiss M, Schmidt J, Eich C et al. Recommendations for the prevention and treatment of the unexpectedly difficult airway in pediatric anesthesia. Anaesth Intensivmed 2011; 52: S54-S63
- Cote CJ, Hartnick CJ. Pediatric transtracheal and cricothyrotomy airway devices for emergency use: which are appropriate for infants and children? Paediatr Anaesth 2009; 19 Suppl 1: 66-76, DOI: 10.1111/j.1460-9592.2009.02996.x
- Navsa N, Tossel G, Boon JM. Dimensions of the neonatal cricothyroid membrane – how feasible is a surgical cricothyroidotomy? Paediatr Anaesth 2005; 15: 402-406
- Johansen K, Holm-Knudsen RJ, Charabi B et al. Cannot ventilate-cannot intubate an infant: surgical tracheotomy or transtracheal cannula? Paediatr Anaesth 2010; 20: 987-993, DOI: 10.1111/j.1460-9592.2010.03417.x
- Disma N, Asai T, Cools E et al. Airway management in neonates and infants: European Society of Anaesthesiology and Intensive Care and British Journal of Anaesthesia joint guidelines. Br J Anaesth 2024; 132: 124-144, DOI: 10.1016/j.bja.2023.08.040
- Holm-Knudsen RJ, Rasmussen LS, Charabi B et al. Emergency airway access in children – transtracheal cannulas and tracheotomy assessed in a porcine model. Pediatric Anesthesia 2012; 22: 1159-1165, DOI: 10.1111/pan.12045
- Berger-Estilita J, Wenzel V, Luedi MM et al. A Primer for Pediatric Emergency Front-of-the-Neck Access. A&A practice 2021; 15: e01444, DOI: 10.1213/XAA.0000000000001444
- Kaufmann et al. Development and Prospective Federal State-Wide Evaluation of a Device for Height-Based Dose Recommendations in Prehospital Pediatric Emergencies: A Simple Tool to Prevent Most Severe Drug Errors. Prehosp Emerg Care 2018; 22: 252-259.
- Kaufmann et al. Improving Pediatric Drug Safety in Prehospital Emergency Care-10 Years on. J Patient Saf 2021; 17: e1241-e1246.
- Kaufmann et al. S2k guideline 027/071: “Drug safety in pediatric emergencies”. org 2021