July 1, 2023
Button cells: the danger in your own home
More and more frequently and with increasing damage, children swallow button cells. The incidence of severe injury has increased due to both an increasing prevalence of small batteries and greater energy capacity [1, 2]. Often the battery is held in one place by the electrically stimulated muscle tube esophagus. In addition, the moisture of the mucous membrane leads to the discharge of the button cell with the formation of hydrochloric acid and caustic soda. This results in severe burns, which in turn can lead to the formation of ducts (fistulas) between the esophagus and surrounding tissue. If the fistula develops into the trachea or a blood vessel (e.g. aorta), these can be life-threatening and have a high mortality rate [3]. Life-saving tips The three most important measures to keep damage to a minimum: 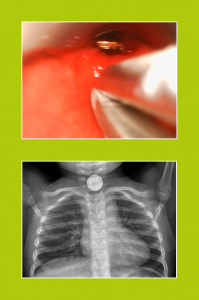
- Prevention through education: Button cells and devices containing them should be kept out of the reach of children. Button cells are round, shiny and encourage children to grab them. Toddlers “explore” things mainly with their mouths. There acidity makes them taste lemony sour, so they are often swallowed rather than spit out!
- Go to hospital immediately : You should let children older than 1 year swallow honey (10 ml every 10 minutes up to six times). Children younger than 1 year of age should drink sucralfate suspension under medical supervision (1g/10 ml, 10 ml every 10 minutes for up to three times).
- Get out fast! We have presented the simplest and fastest method in a prospective intervention study with 100% success rate and excellent feasibility and published it as open access: Under anesthesia (supported by the pediatric anesthesia ruler PädOP), go into the esophageal inlet with a (long) laryngoscope blade. If the button cell can be displayed, recover it with a pair of pliers (e.g. Magill pliers or similar) [4]. This can and should be done by facilities that do not have pediatric endoscopy. Because if it succeeds, the otherwise delayed recovery after lengthy hospital transfer is avoided. If it does not succeed, the transfer to a special center must take place.The procedure presented here saves children’s lives! Details in the PDF of the study at: https://onlinelibrary.wiley.com/doi/full/10.1111/pan.14158
Literature:
- Litovitz, T., et al, Emerging battery-ingestion hazard: clinical implications. Pediatrics, 2010. 125(6): p. 1168-77.
- Lerner, D.G., et al, Mitigating Risks of Swallowed Button Batteries: New Strategies Before and After Removal. J Pediatr Gastroenterol Nutr, 2020. 70(5): p. 542-546.
- Pae, S.J., et al, Battery ingestion resulting in an aortoesophageal fistula. Anesthesiology, 2012. 117(6): p. 1354.
- Kaufmann, J., et al, Rapid and safe removal of foreign bodies in the upper esophagus in children using an optimized Miller size 3 video laryngoscope blade. Paediatr Anaesth, 2021. 31(5): p. 587-593.

